According to a new study shows that a serious condition that can cause the kidneys to suddenly stop working could be treated with existing medicines.
New research findings reveal that a serious condition that can cause the kidneys to suddenly stop working could be treated with existing medicines.
Scientists found that medicines usually used to treat angina and high blood pressure prevented much of the long-term damage to the kidney and cardiovascular system caused by acute kidney injury (AKI). The study, which was conducted in mice, was published on December 14, in the journal Science Translational Medicine.
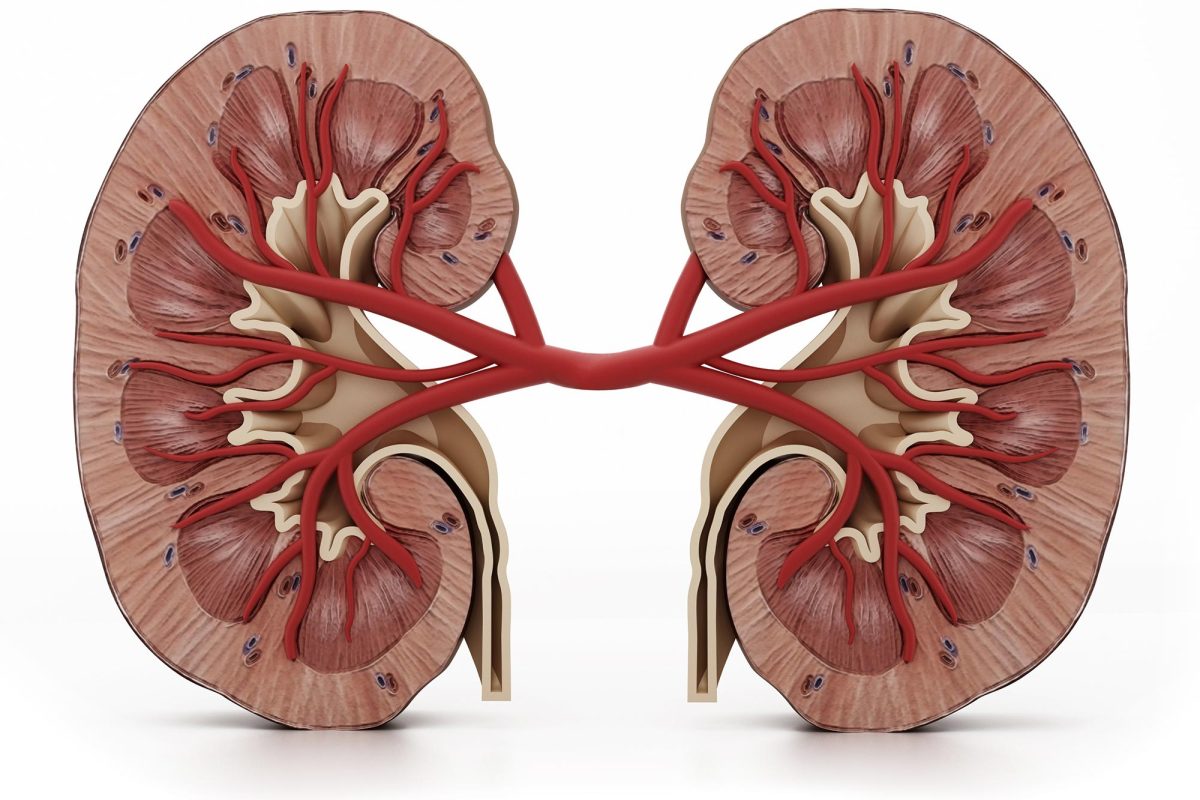
Acute kidney injury (AKI), previously called acute renal failure (ARF), is an abrupt decline in kidney function that develops within 7 days. This condition is indicated by an increase in serum creatinine or a decrease in urine output, or both.
Experts hope the findings will pave the way for improved treatment of AKI – a common condition that occurs in approximately 20 percent of emergency hospital admissions in the UK.
The condition is usually caused by other illnesses that reduce blood flow to the kidney (such as low blood pressure, blood loss, heart attack, or organ failure), or due to toxicity arising from some medicines.
AKI must be treated quickly to prevent death. Even if the kidneys recover, AKI can cause long-lasting damage to the kidneys and the cardiovascular system.
Of those who survive an episode of AKI, 30 percent are left with chronic kidney disease (CKD). The remaining 70 percent that recover full kidney function are at an almost 30-fold increased risk of developing CKD. In time, CKD can result in kidneys that stop working altogether. This is known as kidney failure, end-stage renal disease (ESRD), or end-stage kidney disease (ESKD).
A team from the University of Edinburgh found that patients with AKI had increased blood levels of endothelin – a protein that activates inflammation and causes blood vessels to constrict. Endothelin levels remained high long after kidney function had recovered.
After finding the same increase in endothelin in mice with AKI, experts treated the animals with medicines that block the endothelin system. The medicines – normally used to treat angina and high blood pressure – work by stopping the production of endothelin or by shutting off endothelin receptors in cells.
The mice were monitored over a four-week period after AKI. Those that were treated with the endothelin-blocking medicines had lower blood pressure, less inflammation and reduced scarring in the kidney.
Their blood vessels were more relaxed and kidney function was also improved, compared with untreated mice.
Dr. Bean Dhaun, Senior Clinical Lecturer and Honorary Consultant Nephrologist at the University of Edinburgh’s Centre for Cardiovascular Science, said: “AKI is a harmful condition, particularly in older people and even with recovery it can have a long-term impact on a person’s health. Our study shows that blocking the endothelin system prevents the long-term damage of AKI in mice. As these medicines are already available for use in humans, I hope that we can move quickly to see if the same beneficial effects are seen in our patients.”
Professor James Leiper, Associate Medical Director at the British Heart Foundation, said: “Impaired kidney function that results from acute kidney injury can also increase a person’s chance of developing and dying from heart and circulatory diseases, so it’s vital we find ways to reduce this risk.
“This promising research suggests that widely available medicines could help to tackle the impact of acute kidney injury before it can cause damage and further complications. While further studies will be needed to demonstrate whether this treatment is safe and effective for patients, this early research is an encouraging first step.”
Reference: “Endothelin blockade prevents the long-term cardiovascular and renal sequelae of acute kidney injury in mice” by Alicja Czopek, Rebecca Moorhouse, Peter J. Gallacher, Dan Pugh, Jessica R. Ivy, Tariq E. Farrah, Emily Godden, Robert W. Hunter, David J. Webb, Pierre-Louis Tharaux, David C. Kluth, James W. Dear, Matthew A. Bailey and Neeraj Dhaun, 14 December 2022, Science Translational Medicine.
DOI: 10.1126/scitranslmed.abf5074
The study was published on December 14, 2022, in the journal Science Translational Medicine. It was funded by the Medical Research Council and the British Heart Foundation.
Share your story or advertise with us: Whatsapp: +2347068606071 Email: info@newspotng.com