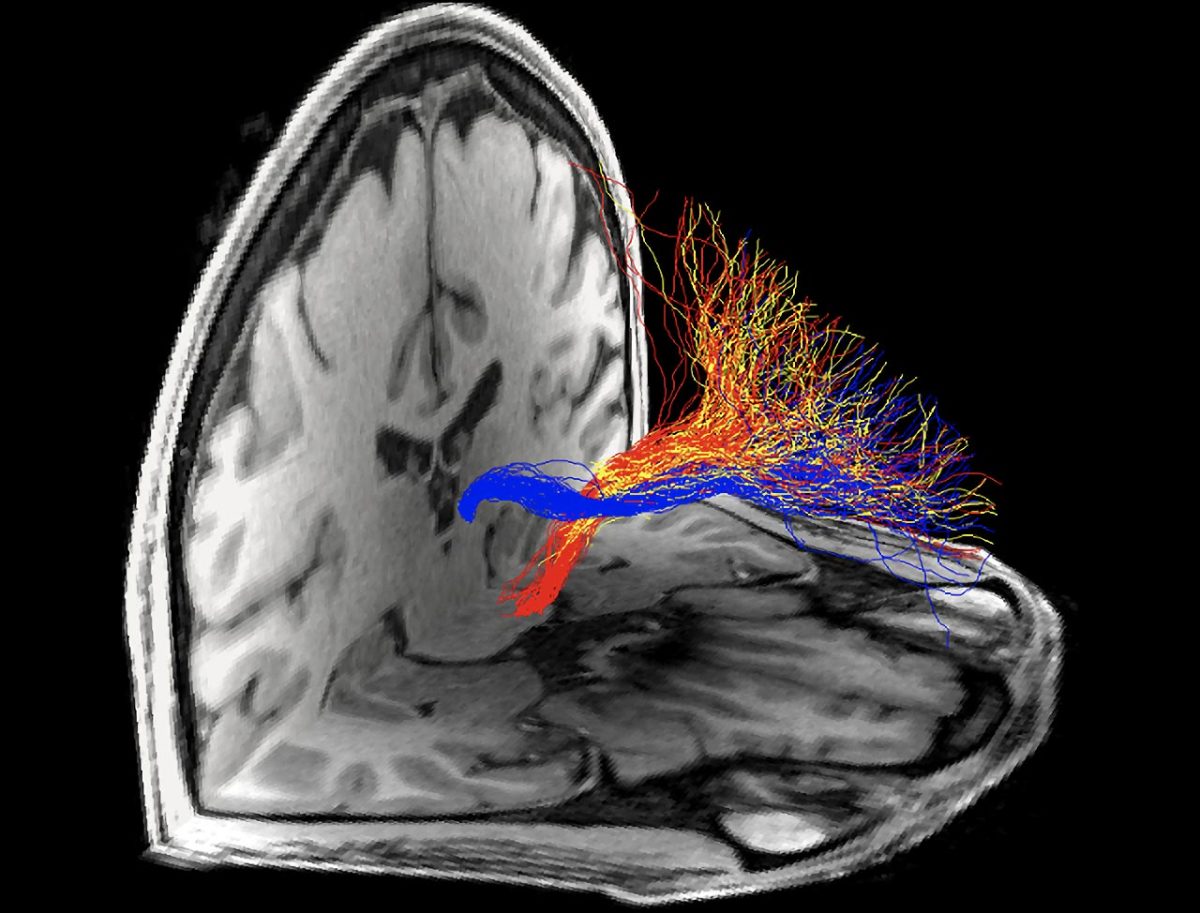
A new study reveals that impairment in a specific brain circuit in people is linked to addiction to cocaine or heroin. Credit: Mount Sinai Health System
According to a new study, white matter in the brain that was previously implicated in animal studies has now been suggested to be specifically impaired in the brains of people with addiction to cocaine or heroin. The research, which was published on October 6 in the journal Neuron, was conducted by scientists from the Icahn School of Medicine at Mount Sinai and Baylor College of Medicine.
In the study, investigators examined the connectivity of the tract between the prefrontal cortex (PFC), a brain region critical for regulating higher-order executive functions, and the habenula, a region that plays a critical role in reward and reward-associated learning. In animal models of addiction, the habenula has emerged as a key driver of drug-seeking behaviors. Specifically, signaling from the PFC to the habenula is disrupted in rodent cocaine addiction models, implicating this PFC-habenula circuit in withdrawal and cue-induced relapse behaviors. However, until now, the PFC-habenula path has remained poorly understood in the human brain. Furthermore, its involvement in the neuropathological effects of drugs other than cocaine has not been previously explored.

Structural connections with the prefrontal cortex modeled from targeted nuclei in the subcortex (blue: habenula, yellow: anterior thalamus, red: ventral tegmental area) using diffusion MRI tractography. Microstructural properties of the habenula tract were uniquely reduced in individuals with cocaine or heroin use disorder. Results highlight the potential specificity of distinct prefrontal cortical connections to the neuropathology of drug addiction. Credit: Mount Sinai Health System
For the first time in the human brain, a team of scientists used diffusion magnetic resonance imaging (MRI) tractography to investigate the microstructural features of the PFC-habenula circuit in people with cocaine or heroin addiction compared to healthy control participants. Diffusion MRI tractography uses noninvasive brain imaging to model fiber bundles in the living human brain.
The researchers were led by Rita Z. Goldstein, PhD, and Junqian Xu, PhD. Dr. Goldstein is the Mount Sinai Professor in Neuroimaging of Addiction and Director of the Neuroimaging of Addictions and Related Conditions Research Program at Icahn Mount Sinai. Dr. Xu is Associate Professor of Radiology, and Psychiatry, at Baylor College of Medicine.
“In addition to identifying microstructural differences, specifically reduced coherence in the orientation of the white matter fibers in the cocaine-addicted group that comprised both current cocaine users and those with short-term abstinence, we extended results beyond cocaine (a stimulant) to heroin (an opioid), suggesting that abnormalities in this path may be generalized in addiction,” said Sarah King, who led the analyses and is first author of the paper. “Importantly, we found that across all addicted individuals, greater impairment was correlated with earlier age of first drug use, which points to a potential role for this circuit in developmental or premorbid risk factors.” King is a PhD student in Neuroscience in the Graduate School of Biomedical Sciences at Icahn Mount Sinai.
The results advance ongoing research in the field by targeting a previously unexplored circuit in the pathophysiology of addiction in humans, where deficits may predispose an individual to both the development of drug addiction and to relapse and which may be potentially amenable for individually tailored treatment or prevention efforts.
Reference: “Prefrontal-habenular microstructural impairments in human cocaine and heroin addiction” by Sarah G. King, Pierre-Olivier Gaudreault, Pias Malaker, Joo-won Kim, Nelly Alia-Klein, Junqian Xu and Rita Z. Goldstein, 6 October 2022, Neuron.
DOI: 10.1016/j.neuron.2022.09.011
Share your story or advertise with us: Whatsapp: +2347068606071 Email: info@newspotng.com